What is patient-focused care and how is it different?
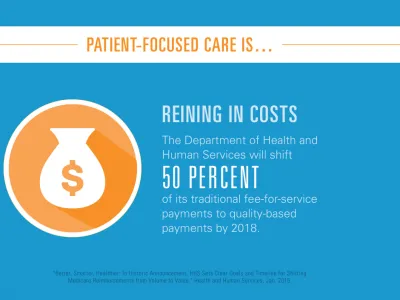
The U.S. healthcare system produces extraordinary medical advances and delivers some of the best care in the world—but it does so with inefficiencies and complexities that drive up costs and can even harm patients. Our current system of paying for medical care rewards doctors, hospitals and medical professionals for the volume of services they provide. This tilts the system toward even more procedures and interventions and pushes up costs without necessarily improving patients’ health.
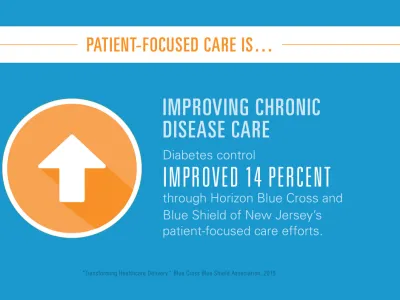
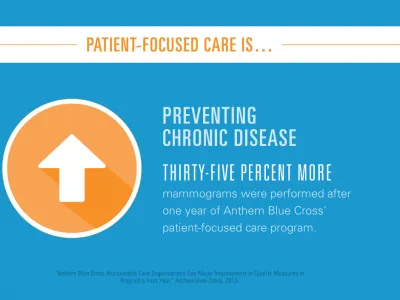
Yet we know that when we focus on our patients, they get healthy faster and stay healthy longer. Patient-focused, or patient-centered, care is high-quality, comprehensive and safe.
A patient-focused model of care bases a practitioner’s compensation on patient outcomes. Doctors earn more when they deliver high-quality care that’s based on helping people stay healthy.
As with any transition, moving to a patient-centered care system requires collaboration. Public and private sector payers, hospitals, doctors and nurses must work together with the goal of ensuring that every patient receives high-quality care.
How is it being implemented?
There are many new and exciting models of care that are being tested—and are already demonstrating solid results. Among the most common are Patient-Centered Medical Homes (medical home) and Accountable Care Organizations (ACOs).
A medical home is a team of medical professionals—primary care doctors, specialists, nurses, therapists, pharmacists and care coordinators—who work together to meet a patient’s varied health needs. The team coordinates all levels of care, is accessible at all times and employs data to meet the highest standards of safety and quality. Medical homes form strong relationships with their patients and help them define and meet their health needs. Think of them like the family doctors of decades ago—supported by the modern technology and data-driven insights available today.
An ACO is a group of doctors, nurses and other medical professionals that works in collaboration to care for their patients. The quality of care and the patients' health outcomes determine how much the team is paid.
Where is patient-focused care happening?
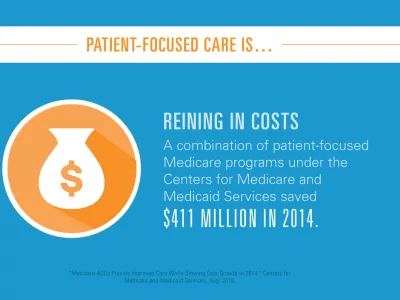
Private and public sector partners across the healthcare industry are embracing patient-focused care. For example, the Vermont Blueprint for Health program, pioneered by the state's government, uses medical homes, practice facilitators and community health teams to coordinate care and provide health coaching, among other services. From 2008 to 2013, the program generated $104.4 million in annual savings. For every $1 million spent on the program, medical expenditures decreased by $5.8 million.
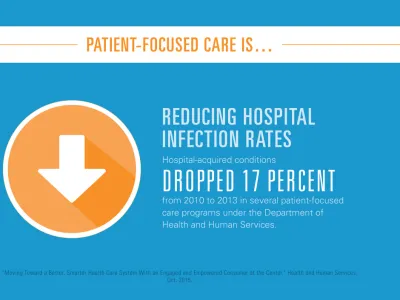
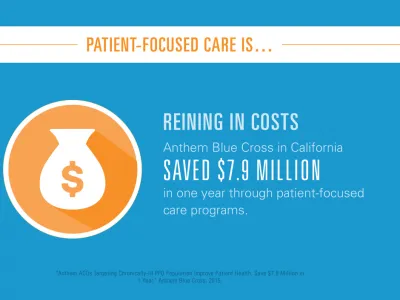
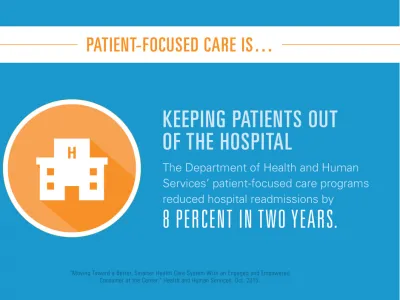
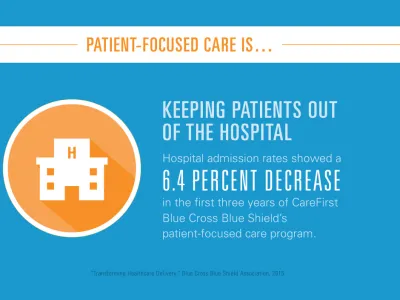
Blue Cross and Blue Shield companies are leading more than 700 patient-focused care programs and have already demonstrated reductions in unnecessary emergency department visits, hospital admissions, readmission rates, and hospital infections. For instance, CareFirst Blue Cross Blue Shield reduced hospital admissions by 6.4 percent in the first three years of its medical home, and lowered costs by $267 million. Another plan, Anthem Blue Cross in California, lowered costs by almost $8 million through its ACO.
What's the government's role?
Since all patients have different needs—and local healthcare systems are all distinct—a “one size fits all” approach won't work. Payers, doctors and employers must work together to discover the best way to care for their unique populations and pay doctors. Policymakers can support the transition to a patient-centered model by giving the healthcare system a framework to measure patient outcomes and reward effective doctors. Read more on advancing patient-focused care.
What can employers do?
Employers can harness the power of data to better understand their workers’ healthcare needs. Data provides insight to help determine the most effective, efficient and affordable care.
In a complicated healthcare system, how do you measure quality?
We live in an era of unparalleled access to data. That enables us to determine the key metrics to measure health outcomes. Is care prompt and cost-effective? Do patients recover quickly? Do patients remain healthy? And, most importantly, are patients satisfied? Quality metrics empower us to deliver quality care.