Health care costs are rising. We’ve got solutions
A roadmap to lowering costs by nearly $1 trillion
Premiums rise when care and medication costs climb. And both are higher than ever. But we have a plan — one that could save $1 trillion over time.
Americans feel the impact of higher costs. Some delay care. Some cut pills in half. Many reduce discretionary spending. These are consequences of a health care affordability crisis. The causes are clear:
- Medical prices have grown 40% faster than inflation since 2000.
- Drug spending jumped 10% in 2024.
Patients now need more intensive — and expensive — care. On top of that, demand for health care continues to surge, driving higher spending.
All of this leads to higher premiums and higher out-of-pocket costs for patients.
Our roadmap tackles the affordability crisis. The Blue Cross Blue Shield Association (BCBSA) is taking action with a plan for policymakers to improve competition, lower prescription drug cost and prioritize high-quality care.
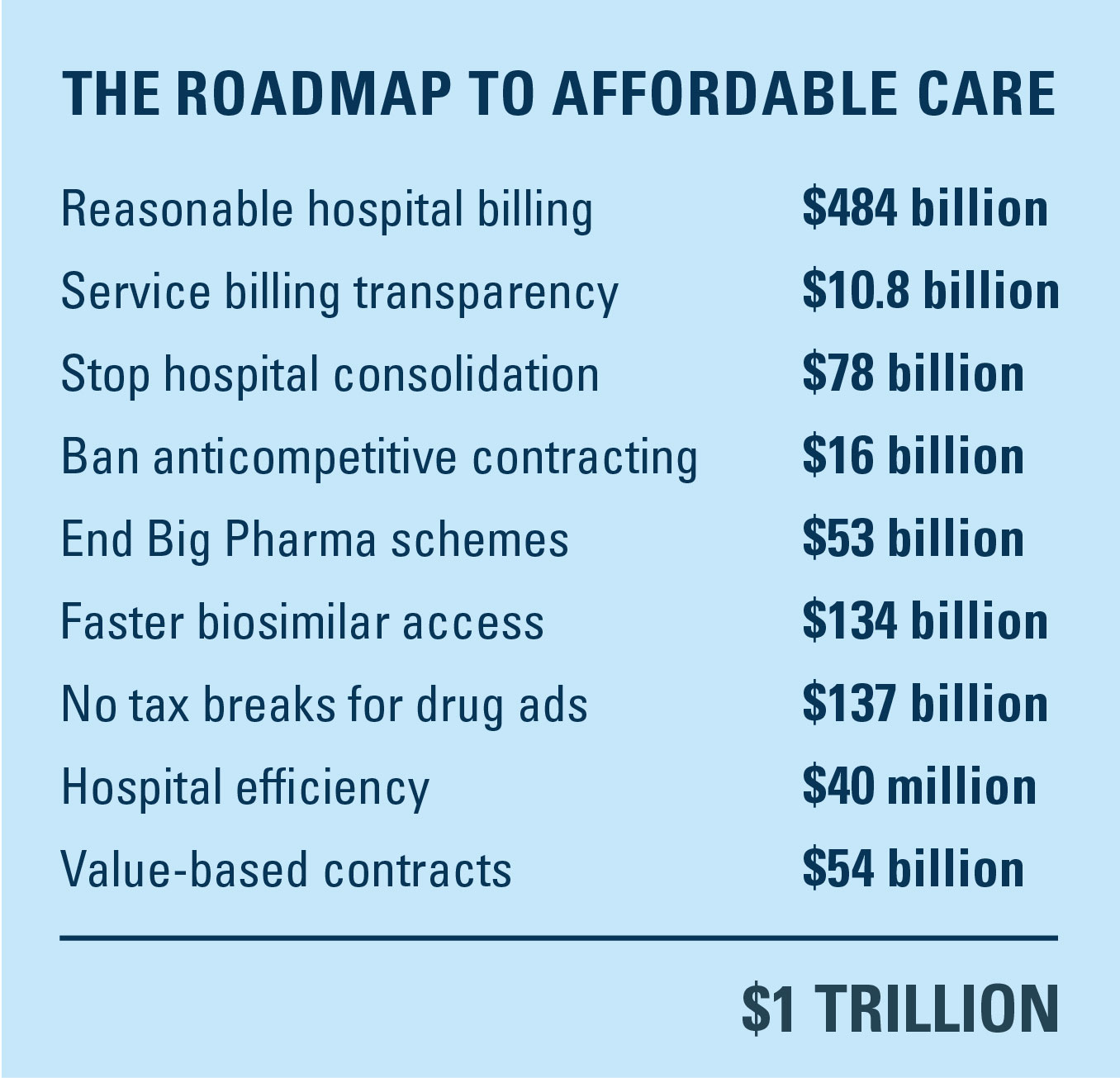
The trillion-dollar prescription for affordability
The latest economic analysis shows that BCBSA's 2025 Affordability Solutions for the Health of America could deliver $1 trillion in savings. Yes, trillion with a T.
Protecting patients from unfair hospital practices
Corporate hospital systems drive up costs and limit patient choice. Our solutions restore fairness, transparency and affordability for patients.

End unreasonable markups by corporate hospital systems
The problem: Corporate hospital systems are taking over smaller practices and prioritizing profits over patients. After the takeover, you often get the same care in the same location from the same doctors, but at much higher prices. A simple name change, from doctor’s office to hospital outpatient department, means they can now charge 3x more for a routine X-ray.
The solution: Implement fair and reasonable hospital billing. BCBSA's approach — ending unreasonable markups by corporate hospital systems and adopting site-neutral Medicare payments.
Policy action:
- Expand site-neutral policies in Medicare to drive care toward lower-cost settings. One proposal would eliminate the exemption that currently lets certain hospital off-campus outpatient departments (HOPDs) avoid these requirements.
- Apply site-neutral policies to Ambulatory Payment Classifications across sites of care. Align rates for services provided in off-campus HOPDs and ambulatory surgical centers with lower-cost settings.
In 2025, Centers for Medicare & Medicaid Services finalized a site-neutral solution that will save Medicare beneficiaries $70 million in lower out-of-pocket costs in 2026.

Ensure transparent, appropriate billing for health care services
The problem: Hospital systems often use a single national provider identifier (NPI) for both on-campus and off-campus sites of service. This makes it difficult for insurers to identify when services are rendered in non-hospital settings, where they would typically pay a lower rate.
The solution: Prevent hospitals from obscuring where care is delivered by requiring hospital billing and claims forms to accurately reflect where care is delivered. This clarity allows insurers to apply the correct payment rate and patient cost sharing.
Policy action:
- Require off-campus hospital sites to obtain a different NPI from the main hospital campus and submit claims using the appropriate form (Fair Billing Act).

Combat hospital consolidation that leads to higher prices and fewer choices for patients
The problem: Hospital consolidation reduces competition and raises prices — by 20% on average. About 80% of hospital markets are considered highly consolidated, giving large systems outsized power to raise prices. Cross-market mergers are on the rise and rural areas face a growing crisis.
The solution: Crack down on corporate hospital systems taking over smaller, local hospitals to drive out competition and drive up prices.
Policy action:
- Encourage the FTC to review and enforce antitrust laws regarding physician practice consolidation, including physician practice mergers and hospital acquisitions of physician practices.
- Extend the FTC’s jurisdiction to review and regulate anti-competitive behavior among nonprofit health care providers by amending the Federal Trade Commission Act.
- Require HHS or GAO to conduct annual state-level studies of reported vertical and horizontal mergers of providers to inform future policymaking.

Stop hospital contracting practices that allow monopoly power and raise costs
The problem: Corporate hospital systems can exploit their size and market power to impose anticompetitive contracting terms with employers and insurers that reduce patient access, drive up costs and allow hospital administrators to pad their profits.
The solution: Congress should push back on anti-tiering provisions in payer-provider contracts to address rising costs. Lawmakers can do this by limiting terms that force insurers to treat every hospital within a system the same, regardless of cost or performance, and by preserving insurers’ ability to design benefits that guide patients toward more affordable, higher-quality in-network hospitals.
Policy action:
- Prohibit anti-competitive contracting practices by banning hospitals from requiring contract terms that compel payers to include all affiliated hospitals in a plan’s network (“all-or-nothing”) and restrict benefit designs that steer patients to lower-cost, higher-quality in-network hospitals (“anti-tiering”).
Affordable medicines: Closing pharma loopholes that delay patient access
Pharma companies exploit loopholes to maintain monopolies and keep drug prices high. These solutions increase competition, speed access to affordable medicines and lower costs for patients.

Ending big pharma roadblocks to affordable medicines
The problem: Drug companies use schemes like patent thicketing, where they file dozens of patents to extend their drug’s monopoly and delay access to lower-cost, equally effective generic drugs.
For example, the blockbuster drug Humira’s original patent should have expired in 2016, but 75 additional patents extended its monopoly by 18 years and protected its massive profitability.
The solution: Stop Big Pharma’s unfair business practices with more market competition, more patient choices and lower costs for consumers.
Policy action:
- Prevent pharma patent gaming. Limit the number of patents in infringement claims against biosimilar applicants (Affordable Prescriptions for Patients Act).
- End anticompetitive product hopping. Prohibit switches from a brand drug to a similar, newly patented brand drug to delay competition. For example, changing from a twice-daily pill to a once-daily extended-release version solely to extend exclusivity (Drug Competition Enhancement Act).
- Ban pay for delay backroom deals that compensate competitors to postpone generic or biosimilar entry. Recent research estimates pay for delay settlements drive up drug costs by nearly $12 billion per year — $3 billion of that amount comes out of patients’ pockets (Preserve Access to Affordable Generics and Biosimilars Act).
- Streamline patient access to biosimilars. Remove switching study requirements for interchangeability designation that allows pharmacists to dispense lower-cost biosimilars (Biosimilar Red Tape Elimination Act).

Level the playing field with shorter biologic exclusivity
The problem: Biologic drugs offer breakthrough treatments, but long exclusivity periods — 12 years of monopoly pricing compared to much shorter timelines for traditional drugs. This keeps prices high and limits patient access.
The solution: Shorten the 12-year exclusivity period for biologics to seven years, the same as for traditional drugs, allowing more affordable biosimilars to enter the market sooner.

Eliminate tax deductions for drug advertisements
The problem: Drug companies get a tax break for all those direct-to-consumer (DTC) ads on your TV. The U.S. is one of only two countries that allow DTC ads, which drive overuse of costly drugs, even when lower-cost alternatives exist. Advertised drugs account for more than half (58%) of Medicare drug spending, and research shows a 10% increase in DTC spending leads to a 5.4% increase in product revenue.
The solution: Eliminate the ability of drug manufacturers to receive tax deductions for expenses associated with DTC ads.
Increase 340B program accountability
The problem: The number of 340B covered entities has increased 228% from 2012 to 2022. While BCBSA supports the 340B program to help low-income patients receive affordable medications, this trend raises concerns about transparency and oversight.
The solution: Promote greater stewardship and accountability of the program.
Policy action:
- Require 340B claims modifiers on all medical and pharmacy benefit claims, allowing health plans to more accurately file rates and bids, and support Medicaid managed care organizations in complying with duplicate discount requirements.
- Mandate hospital public disclosure of how 340B savings are used to benefit communities thereby supporting policymaker oversight and program integrity efforts.
Aligning quality, access and affordability for better patient outcomes
Aligning quality, access and affordability is key to better outcomes and lower costs. Our solutions drive value-based care, expand proven models and remove barriers to telehealth to deliver billions in savings and better health for all.

Encourage hospital efficiency with greater transparency
The problem: Hospital administrative costs are rising faster than inflation and faster than the cost of patient care. From July 2023 to June 2024, hospital costs jumped 6.9%, more than double the inflation rate during that time, and from 2019–2020, administrative costs grew 6.2%, while clinical costs barely moved.
The solution: Require hospitals to report how much they spend on administration compared to care. This solution would have hospitals publicly report administrative costs as a share of revenue, measured against a federal benchmark. Making these costs transparent, without punitive fines, could encourage hospitals to operate more efficiently.

Boost provider participation in value-based contracts
The problem: Too many health care providers still get paid based on the number of services they deliver, not the quality of care they provide to patients. While Medicare has created programs to reward better outcomes, most providers aren’t required to participate. That means billions in potential savings and better health outcomes are left on the table.
The solution: Require provider systems to join value-based contracts (VBC) that share both savings and risk, making this a condition for Medicare participation. These “two-sided” agreements create stronger incentives to improve care and control costs. This BCBSA solution would apply to fee-for-service (FFS) Medicare and Medicare Advantage (MA). With over half of all Medicare beneficiaries enrolled in MA, the impact is significant.
Policy action:
- Require VBC participation for Medicare and Medicare Advantage providers. Mandate FFS Medicare and MA providers join two-sided VBC arrangements to improve health outcomes and reduce overall costs. Include low-interest loans for independent, rural and primary care providers to support the transition.
- Provide targeted loans for VBC infrastructure. Offer loans to help providers invest in population health tools and data analytics to transition from FFS. Providers must commit to multi-year VBC participation and repay loans after achieving savings.
- Offer dual-track hospital payments to reward VBC adoption. To help incentivize VBC arrangements, increase FFS payment updates for hospitals in two-sided risk with MA plans. Hospitals not assuming risk would be ineligible for these increased payments, ensuring incentives align with quality over volume.
Increase adoption of multi-payer CMMI models
The problem: Many models from the Center for Medicare & Medicaid Innovation (CMMI) have focused exclusively on Medicare and Medicaid. To expand the reach of CMMI, the agency should focus on models with multi-payer alignment among Medicare, Medicaid and private insurers, when feasible, to support a shared standard for innovation in quality, payment and reporting. Multi-payer models have the greatest potential for success by maximizing provider participation, reducing administrative burden, enhancing population health and supporting financial sustainability.
The solution: Increase adoption of CMMI models with multi-payer alignment to drive consistency across markets and support systemic transformation.
Policy action:
- Test and expand models with direct accountability for health outcomes and costs in FFS, MA, Medicaid and commercial insurers.
- Align quality measures across payers, when appropriate, to reduce duplication and minimize provider administrative burden.
Remove barriers to appropriate use of telehealth
The problem: Outdated regulations and statutory limits threaten continued use of telehealth, which proved its value during the pandemic by expanding access to care, especially in underserved communities and with specialty physicians.
The solution: Remove long-standing barriers that restrict telehealth in Medicare. Policymakers should support flexibility in coverage and avoid prescriptive mandates that undermine accessibility and innovation.
Policy action:
- Permanently remove barriers such as statutory geographic and originating site restrictions in Medicare.
- Prevent federal and state mandates related to reimbursement, site-specific use, prior visit requirements or specific technology use.
For more information on what it takes to bring down the cost of health care, read the full 2025 report from Harmonic Consulting, Dare Actuarial Consulting, and Helse Consulting Group.
The latest in health care, delivered.
Subscribe to stay in the know on health care industry news and insights.