Connecting Your Employees to Higher-Performing Healthcare
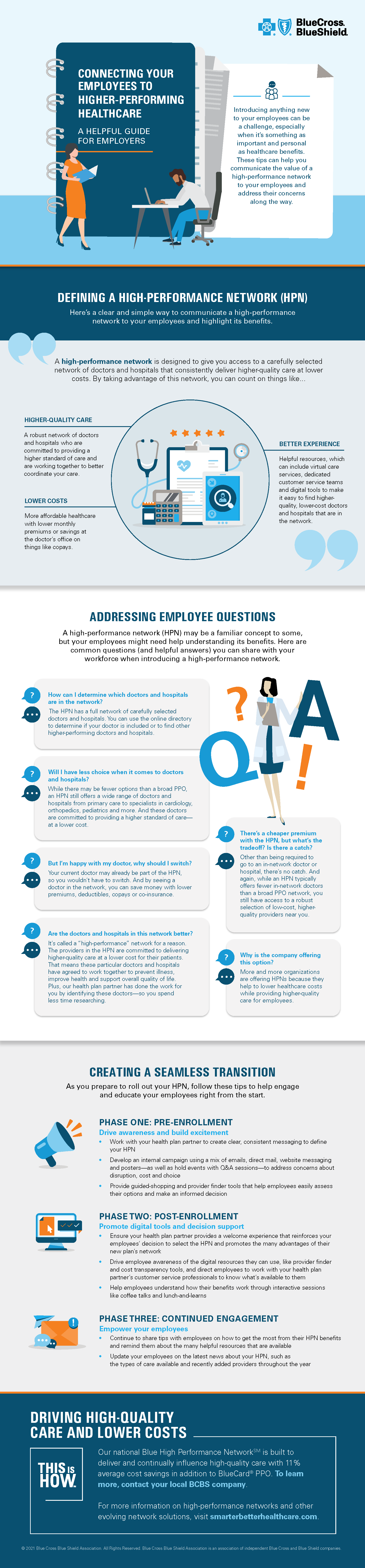
Introducing anything new to your employees can be a challenge, especially when it's something as important and personal as healthcare benefits. These tips can help you communicate the value of a high-performance network to your employees and address their concerns along the way.
Defining a High-Performance Network
Here's a clear and simple way to communicate a high-performance network to your employees and highlight its benefits. A high-performance network is designed to give you access to a carefully selected network of doctors and hospitals that consistently deliver higher-quality care at lower costs. By taking advantage of this network, you can count on things like:
Higher-quality care
A robust network of doctors and hospitals who are committed to providing a higher standard of care and are working together to better coordinate your care.
Lower costs
More affordable healthcare with lower monthly premiums or savings at the doctor's office on things like copays.
Better experience
Helpful resources, which can include virtual care services, dedicated customer service teams and digital tools to make it easy to find higher-quality, lower-cost doctors and hospitals that are in the network.
Addressing Employee Questions
A high-performance network may be a familiar concept to some, but your employees might need help understanding its benefits. Here are common questions (and helpful answers) you can share with your workforce when introducing a high-performance network.
Question: How can I determine which doctors and hospitals are in the network? Answer: The HPN has a full network of carefully selected doctors and hospitals. You can use the online directory to determine if your doctor is included or to find other higher-performing doctors and hospitals.
Question: Will I have less choice when it comes to doctors and hospitals? Answer: While there may be fewer options than a broad PPO, an HPN still offers a wide range of doctors and hospitals from primary care to specialists in cardiology, orthopedics, pediatrics and more. And these doctors are committed to providing a higher standard of care — at a lower cost.
Question: But I'm happy with my doctor, why should I switch? Answer: Your current doctor may already be part of the HPN, so you wouldn't have to switch. And by seeing a doctor in the network, you can save money with lower premiums, deductibles, copays or co-insurance.
Question: Are the doctors and hospitals in this network better? Answer: It's called a "high-performance" network for a reason. The providers in the HPN are committed to delivering higher-quality care at a lower cost for their patients. That means these particular doctors and hospitals have agreed to work together to prevent illness, improve health and support overall quality of life. Plus, our health plan partner has done the work for you by identifying these doctors — so you spend less time researching.
Question: There's a cheaper premium with the HPN, but what's the tradeoff? Is there a catch? Answer: Other than being required to go to an in-network doctor or hospital, there's no catch. And again, while an HPN typically offers fewer in-network doctors than a broad PPO network, you still have access to a robust selection of low-cost, higher-quality providers near you.
Question: Why is the company offering this option? Answer: More and more organizations are offering HPNs because they help to lower healthcare costs while providing higher-quality care for employees.
Creating a seamless transition
As you prepare to roll out your HPN, follow these tips to help engage and educate your employees right from the start.
Phase one: Pre-enrollment
Drive awareness and build excitement
Work with your health plan partner to create clear, consistent messaging to define your HPN.
Develop an internal campaign using a mix of emails, direct mail, website messaging and posters — as well as hold events with Q&A sessions — to address concerns about disruption, cost and choice.
Provide guided-shopping and provider finder tools that help employees easily assess their options and make an informed decision.
Phase two: Post-enrollment
Promote digital tools and decision support
Ensure you health plan partner provides a welcome experience that reinforces your employees' decision to select the HPN and promotes the many advantages of their new plan's network.
Drive employee awareness of the digital resources they can use, like provider finder and cost transparency tools, and direct employees to work with your health plan partner's customer service professionals to know what's available to them.
Help employees understand how their benefits work through interactive sessions like coffee talks and lunch-and-learns.
Phase three: Continued engagement
Empower your employees
Continue to share tips with employees on how to get the most from their HPN benefits and remind them about the many helpful resources that are available.
Update your employees on the latest news about your HPN, such as the types of care available and recently added providers throughout the year.
Driving high-quality care and lower costs
Our national Blue High Performance Network is built to deliver and continually influence high-quality care with more than 11 percent average cost savings in addition to BlueCard PPO. To learn more, contact your local BCBS company. For more information on high-performance networks and other evolving network solutions, visit smarterbetterhealthcare.com.
