Massachusetts experiment to decrease health care spending is working
An eight year experiment delivers savings
Doctors involved in a Blue Cross Blue Shield of Massachusetts (BCBSMA) payment innovation program have managed to slow health care spending and improve quality for their patients.
What’s more, four key quality measures - meaning outcomes for patients - improved for patients in these doctors’ organizations more than they did for patients across New England and the nation.
That’s the recent conclusion from researchers from Harvard Medical School, who have been tracking how BCBSMA’s statewide effort to transform the way doctors are paid (called the “Alternative Quality Contract,” or AQC) is affecting health care spending and quality since researchers began studying the program eight years ago.
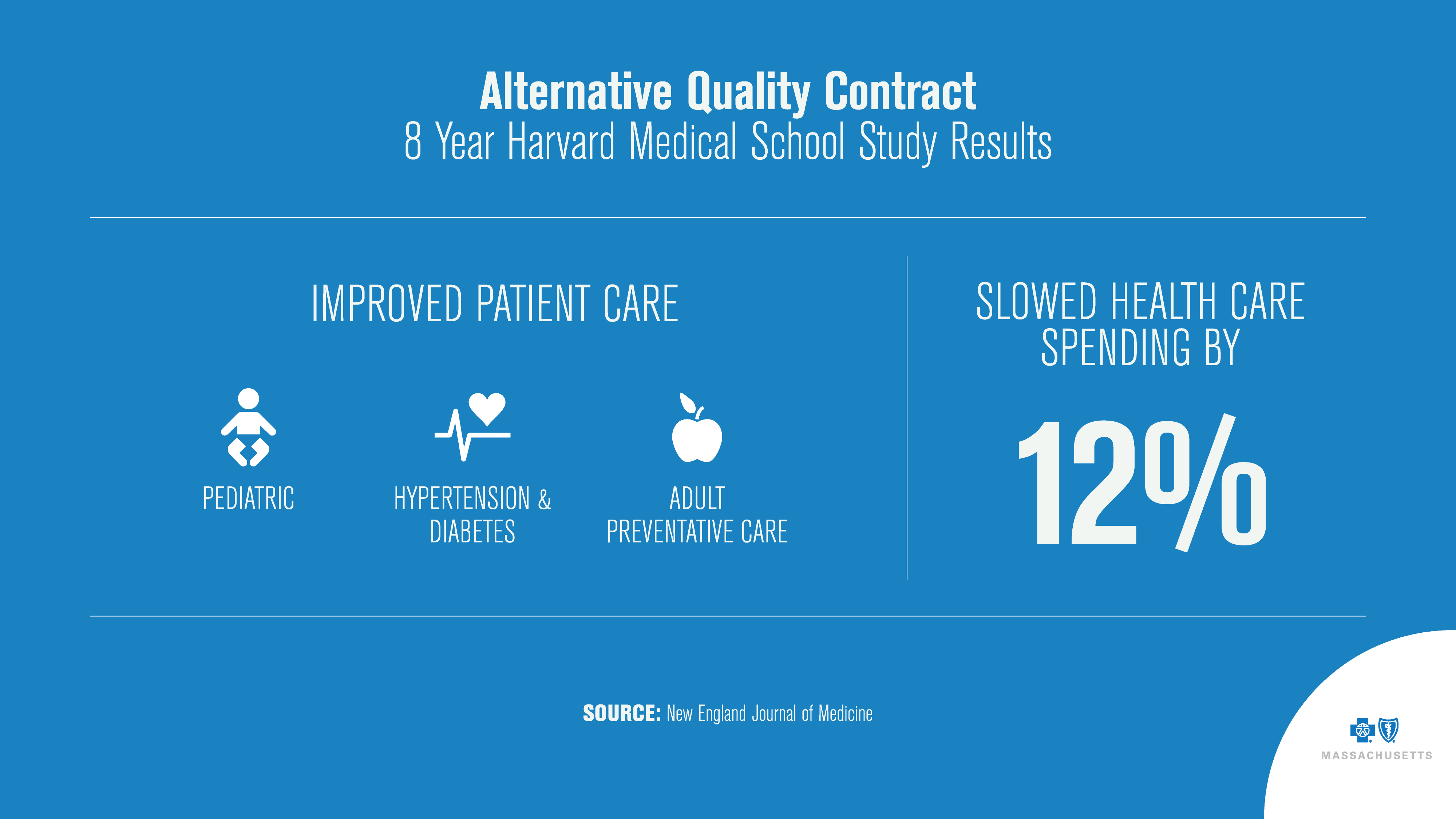
Writing in the New England Journal of Medicine, scientists found that between 2009-2016 “the increase in the average annual medical spending on claims for the enrollees in organizations that entered the AQC in 2009 was $461 lower per enrollee, [or] an 11.7% relative savings on claims.” The study also found improved quality of care across several measures compared to national averages in the areas of diabetes and high blood pressure, for example.
Why payment reform – like the AQC – matters to patients
The AQC gives doctors the flexibility to spend a “pot” of money the way they think is best for patients, including on care management, supportive social services or home care. Doctors can use the money to help patients prevent costly complications from chronic disease, or by avoiding unnecessary services, like duplicative testing or imaging. It’s the opposite of traditional fee-for-service payment models.
Expanding the AQC Model to benefit more patients
For the first time, BCBS Massachusetts has expanded its AQC payment model to an independent nonprofit physician practice, Atrius Health, to care for BCBS Massachusetts’ members. The practice is taking on the full risk (being accountable for cost and quality of care) for more than 130,000 BCBS Massachusetts members.
Here’s what that means: a target amount is set for patient care; what it doesn’t spend, the practice can keep and reinvest in services for patients. If the overall costs of care for their members goes over the target, the physician practice is responsible for making up the difference. That aligns incentives to keep patients healthy, spending on quality, not quantity.
BCBS Massachusetts has also signed a longer-term arrangement with Atrius that provides time to truly prove out the model, says Dr. Steven Strongwater, president and CEO of Atrius Health. And BCBS Massachusetts will help the process by sharing secure medical claims data to identify opportunities for improvement in patient care.
Both health plan and physician group hope not only to eliminate unnecessary health care costs but improve the overall health of their members. “The focus on managing quality and cost as well makes it possible to improve outcomes and lower the total cost of care,” says Strongwater.
Another benefit for BCBSMA members: the partnership aims to create a health care experience for patients that’s simpler and easier to navigate because care and health care coverage are more integrated.
Learn how other BCBS companies are tackling affordability for their members.
Blue Cross Blue Shield of Massachusetts
Blue Cross Blue Shield of Massachusetts is an independent licensee of the Blue Cross Blue Shield Association, an association of independent, locally operated Blue Cross and Blue Shield companies.
Learn more about BCBS Massachusetts’ AQC model.
