Upstate New Yorkers may miss preventive care for these surprising reasons

Most preventive care is covered by health insurance—a federal mandate under the Affordable Care Act. However, many Americans are not receiving these covered services. Excellus BlueCross Blue Shield (Excellus BCBS) commissioned a survey to find out why.
The recent Blue Cross Blue Shield, The Health of America Report® on colorectal cancer trends and risk factors found that most commercially insured Americans do not receive preventive care for colorectal cancer as recommended. That is: regular screenings for Americans over age 50, as well as those diagnosed with Crohn's disease or ulcerative colitis.
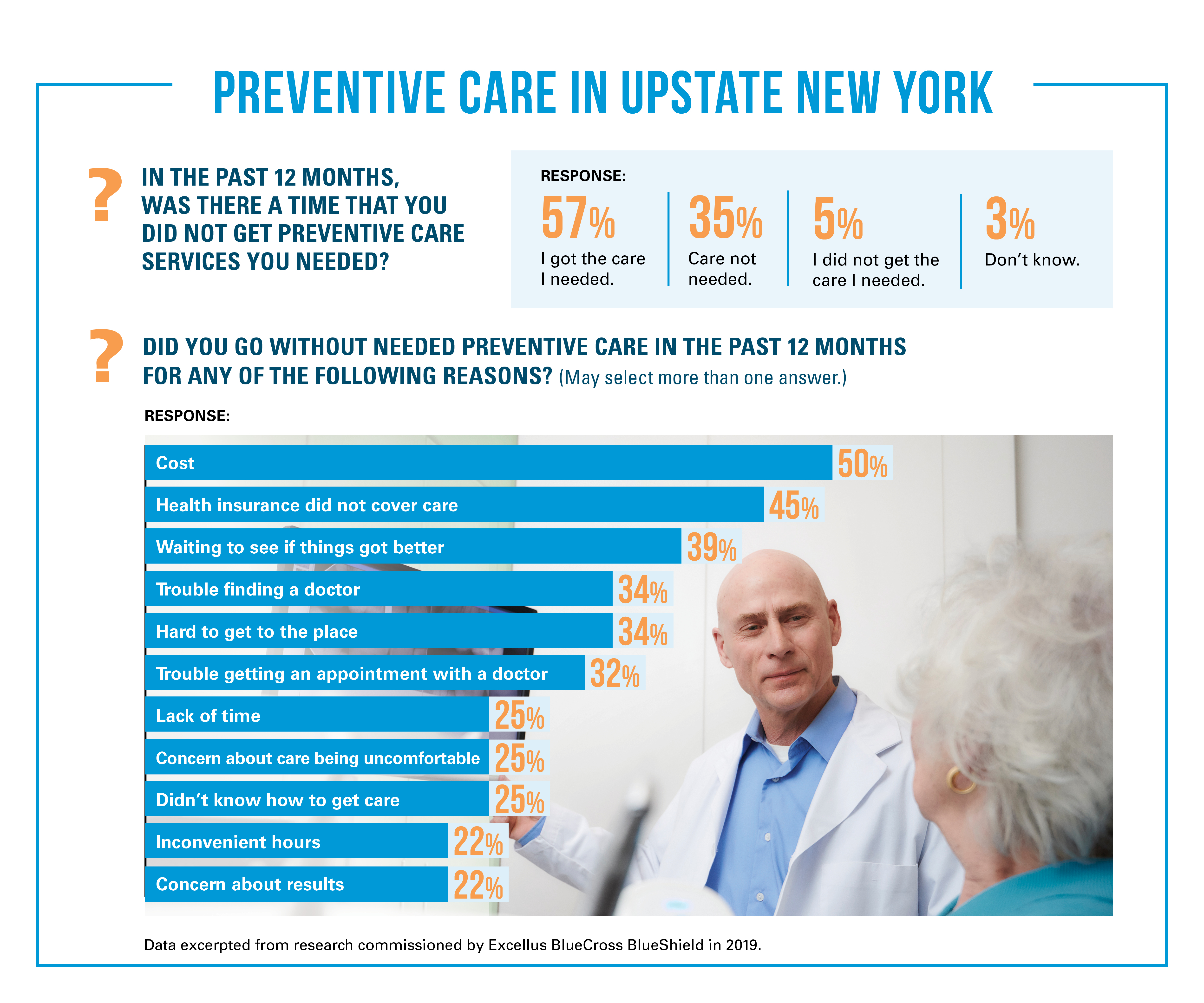
But the problem is bigger than just colonoscopies. Last year, Excellus BCBS commissioned a survey of more than 2,000 adults living in upstate New York. Among other things, the survey asked respondents if they received a preventive screening in the past year and reasons why they might not have.
We spoke with Erika Gruszewski, health research analyst for Excellus BCBS, about the results of the survey and what they mean for the health plan.
When you commissioned this survey, what were you hoping to uncover?
Primarily, we were interested in uncovering barriers to care in upstate New York. We typically do one or two surveys like this each year to learn about our community’s needs and build public awareness campaigns. Our ultimate goal with the survey was to use the findings to improve the health of people living in our communities, , regardless of whether or not they're our customer.
Did any of the findings surprise you?
Yes. We were most surprised that the biggest barriers to preventive care were cost and coverage. Preventive care services, like mammograms and colonoscopies, are generally covered by health insurance plans. So we've taken a step back to ask ourselves, "What do people think preventive care is? How can we break that down and educate our community?" For example, maybe we need to explain the difference between a preventive screening and a diagnostic screening, and what you might get a bill for.
Another surprise was that about 35% of participants said they didn't need any preventive screenings within the last 12 months. Perhaps they don't know what preventive screenings they need, like yearly physicals. Or perhaps they don't know that they're eligible for certain screenings like colonoscopies, for example, if they are at higher risk for developing colon cancer. The responses illuminated potential educational opportunities. We in the industry tend to take for granted the language we use. How we describe these things may not always translate for individual consumers.
What happens now that the survey results are back? What do you do with that information?
After uncovering barriers to care, we shared the results internally. Many of our employees are focused on helping our members navigate the health care system and to get the care that they need. One team, for example, focuses exclusively on women's health. They're responsible for analyzing claims data, member outreach and closing gaps in care. So, they were interested in the same questions we asked in the survey: what are the barriers to preventive screenings? Why are these coming up as issues, and how can we fix that?
Then, we have teams come together and use the results to shape strategies for improving the experience for members and non-members. We go through exercises to map out all the reasons someone might be missing care, including psycho-social barriers and community barriers. Depending on where we land, we may adjust messaging to our members to better educate them. We also build public awareness campaigns to address those barriers via social media, press releases and our community blog, wrapping the member and community in one unified message to improve health across the board.
Hear from an Excellus BCBS employee whose missed colonoscopy was a hard-earned lesson on the value of preventive care.
Excellus BlueCross BlueShield, an independent licensee of the Blue Cross Blue Shield Association, is a nonprofit health plan with 1.5 million upstate New York members. The company's mission is to help people live healthier and more secure lives through access to high-quality, affordable health care. Its products and services include cost-saving prescription drug discounts, wellness tracking tools and access to telemedicine. With more than 3,500 employees, the company is committed to attracting and retaining a diverse workforce to foster innovation and better serve its members. It also encourages employees to engage in their communities by providing paid volunteer time off as one of many benefits. To learn more, visit ExcellusBCBS.com.
